Sleep and pain
Learn how you can encourage sleep to form part of your musculoskeletal pain co-management plan
Last updated: 28 Oct 2023 · 12 min read
Sleep problems and chronic pain seem to go hand in hand. Frequently people with chronic pain find it difficult to fall asleep, or sleep is often disrupted by long night awakenings1. Even if you get a good amount of sleep, you can still feel very tired in the morning as the quality of sleep is often poor. Because of this, it is common for people to want to address sleep as part of pain management.
Having a bad night’s sleep can make you feel more pain sensitive2. Pain and sleep are closely linked and impact each other2. There is a reciprocal relationship where pain during the day affects the quality of that night’s sleep and poor quality sleep increases pain levels the next day1. In fact the latest findings point to sleep affecting pain levels greater than the other way around. So it is important to try and give yourself the best chance of having as good sleep as possible.
Some sleep facts
It is helpful to understand some basic concepts about sleep before we look at what we can do to improve it.
- To drop off to sleep our nervous system has to calm down. If you have chronic pain, you have a much more active nervous system. This can interfere with how quickly you fall asleep and how deep a sleep you get.
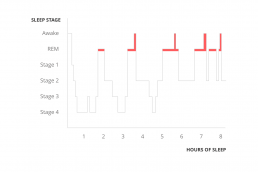
- Know what good sleep looks like. Most people assume that a good night’s sleep involves a steady drop into deep sleep, staying in that deep sleep for most of the night and then gradually moving up into a lighter sleep before you wake. Healthy sleep actually looks quite different from that and instead comes in waves during the night – see the image below.
There are a number of stages of sleep we cycle through:
- We start with stages 1 and 2 which are lighter stages of sleep.
- Then we go down into deeper sleep in stages 3 and 4 sometimes called slow wave sleep.
- We move back up to lighter sleep and then into rapid eye movement or REM sleep. This is where we dream.
- This cycle gets repeated a number of times throughout the night, with more time spent in deep sleep at the beginning of the night and more time spent in lighter stages and dreaming towards the morning.
Notice that after most of the REM stages, we wake up. It is normal to wake up multiple times a night. Most people will roll over and go straight back to sleep without even realising it. When you are in pain, you can wake up and notice your pain. This results in an increase in the activity in your nervous system that then has to calm down all over again to fall back to sleep. If we can help you to fall asleep more quickly initially, many of these same strategies will also help you to fall back to sleep once you wake up during the night.
Pain affects sleep, but a lot of other factors can either improve or impair sleep too1. These are things that you may have more control over and if addressed, can help your sleep3.
How can I improve my sleep?
To help improve your sleeping experience with pain try utilise some sleeping with pain recommendations.
Routine
- Get up at the same time each morning regardless of the sleep you had the night before.
- Go to bed roughly around the same time each night
- Spend half an hour (a very active person may need longer than this) before bed, doing the same things in the same order each night, e.g. get things ready for the next day, have a shower, brush teeth, get into pyjamas then read a book. This helps the body learn to expect sleep and prepare for it. It is important that the last thing that you do in the routine is quiet and relaxing. This is a wind down time.
Only go to bed when you're sleepy
Your sleep goes in waves throughout the night. Your energy levels also go in waves throughout the day. It is important to go to bed when the energy level is in a dip.
- Look for signs of sleepiness
Make the association between “bed” and “sleep” really strong
Your body learns to make associations all the time. We notice that our mouths salivate when we smell our favourite food cooking. We have learnt that soon after smelling food, we will get to eat it. We want to build up the association between bed and sleep, NOT bed and other activities, or bed and stressing about not sleeping, or bed and pain.
- Only use the bed for sleeping (and sex) e. no reading books, watching tv, resting (Find somewhere other than the bedroom to rest during the day)
- That also means no tossing and turning in bed feeling frustrated about being awake.
- If it has been more than 20 mins (roughly) and you have not fallen asleep, get out of bed and do a quiet (non-stimulating) activity, until you feel sleepy and try again.
Relaxation
For the body to drop off to sleep, the nervous system needs to calm down. This can be achieved through involvement in calm non-stimulating activities, or through relaxation. You can find some relaxation techniques in our mindfulness and pain management module.
Relaxation techniques are particularly helpful when you are worried about not being able to sleep or about your pain. However, for it to work well when it is needed it needs to be practiced regularly.
- Practiced regularly to bring down background level of nervous system activation
- Use when dropping off to sleep
Sleep hygiene
This simply means, managing those things that you do during the day that can affect sleep.
- Diet
- avoid heavy, fatty or sugary foods before bed
- avoid caffeine, coffee, coke and chocolate 4 hrs before bed
- have some milk – it is sleep promoting
- Exercise
- Even low levels of exercise are beneficial to sleep
- Don’t exercise within 2-3 hours before going to bed, as it will increase the heart rate and body temperature making it harder to sleep
- Light
The greater the difference between day time light and evening darkness the more “melatonin” the body produces, This is a hormone that promotes sleep
- Reduce light in the bedroom
- Increase sunlight exposure during the day
- Noise
- Ensure a quiet environment
- Temperature
The core body temperature falls as we drop off to sleep.
- A warm shower in the evening is helpful as it will increase the body surface temperature initially, followed by cooling of the core body temperature
Avoid napping
Having a nap during the day will impact the quality of sleep the next night, making it lighter and more easily disrupted. This increases the desire for a nap the next day, creating a vicious cycle.
- Only have a nap during the day as a one off, for a special reason (not routinely).
- If you have to nap, take a short nap in the morning when you will have a lighter sleep and it will have less of an impact on the next night’s sleep.
Download our postcard
We've just created a postcard PDF you can download to share with your patients easily.
Worry, racing thoughts and sleep
When you worry about not sleeping, this increases the activity of your nervous system and will make it more difficult for you to fall asleep. One of the things that can increase our anxiety about not sleeping, is watching the clock. Consider removing the clock from your bedroom. If you need an alarm to wake you, turn the clock around so you can’t actually see the time.
When you can’t sleep, it can also be helpful to remember that this is a natural side effect of pain: fighting against it makes things worse. Accepting you have some sleep difficulties will reduce the distress that you may otherwise feel.
Thoughts that keep churning around in your head can also keep you awake. This often happens at times of high stress. Relaxation here can also help. In particular, mindfulness is a useful technique. This involves practicing letting go of thoughts. When you practice mindfulness, you are not trying to stop having thoughts. You are trying to refocus the brain’s attention on the here and now. As we refocus our attention, the brain lets go of the other thoughts and our body starts to relax. Try a mindfulness exercise using one of our mindfulness meditations.
You may find writing down your thoughts and assure yourself that you will address them in the morning. It can be useful the next day to do your thinking on paper then too. Often our thoughts chase themselves in circles and writing helps to clarify and structure our thinking processes which can help to come up with solutions to our problems.
Mood, anxiety and sleep
Low mood (or depression) and anxiety often start with chronic pain. Both also impact on sleep, but in different ways. Depression can often result in early morning awakening, much earlier than you would like and you cannot get back to sleep. Often it is associated with a racing heart and thoughts that won’t switch off.
For anxiety, it can be difficult to fall asleep initially, with thoughts that don’t want to switch off. If you receive treatment for depression and anxiety, it is likely to have a positive impact on your sleep as well as your mood and pain. You can find some helpful tips for pain and mood management in our approaching pain module.
Professional help
Getting you back into the life that you want involves both managing the impact of your pain and improving your sleep. Some of the techniques used can be difficult to implement. If this is the case, it is good to seek professional help. Psychologists can help with sleep management and can assist with underlying mood and anxiety issues.
If you have breathing related sleep problems such as obstructive or central sleep apnoea, see your GP, the sleep clinic and Sir Charles Gardiner Hospital or one of the many private sleep clinics that are now available.
What about medications and sleep?
Medications can assist in helping you to improve your sleep but are not recommended as a standalone treatment. Many sleep medications are indicated for short term use only as your body builds up tolerance to them.
Sleep problems associated with pain are not often short term problems. Many of them do not give you a sleep that mirrors the natural sleep ‘architecture’, which may mean still feeling tired. In addition, they can also have unhelpful interactions with some pain medications such as opiates.
However, some medicines can be useful for short term use to reset your sleep habits and to break a problematic cycle such as napping. There are some medications that are better for sleep when chronic pain is also there. See your GP to discuss potential medications or take a look at the medicines and procedures pain management module.
Further information
For more clinical information about sleep, we recommend going to Sleep Health Foundation. For information about managing mood and anxiety when you have pain, try our approaching pain management module. You can also find mood help at Beyond Blue or ThisWayUp.
You can find consumer summaries through Cochrane Summaries. Alternatively, if you need to speak to your GP or health care professional, please seek further assistance.
Mindfulness and pain
Approaching pain
Movement with pain
Sleep Health Foundation
Sleep Health Foundation - General sleeping tips
Sleep Health Tracker - Sleep tracker
Ten tips for a good night's sleep
- Kelly GA, Blake C, Power CK, O’Keeffe D, Fullen BM. The association between chronic low back pain and sleep: a systematic review. Clin J Pain. 2011; 27(2):169-81. DOI:10.1097/AJP.0b013e3181f3bdd5. [PubMed]
- Sivertsen B, Lallukka T, Petrie KJ, Steingrimsdottir OA, Stubhaug A, Nielsen CS. Sleep and pain sensitivity in adults. Pain. 2015; 156(8):1433-9. DOI:10.1097/j.pain.0000000000000131.[PubMed]
- Tang NK, Lereya ST, Boulton H, Miller MA, Wolke D, Cappuccio FP. Nonpharmacological Treatments of Insomnia for Long-Term Painful Conditions: A Systematic Review and Meta-analysis of Patient-Reported Outcomes in Randomized Controlled Trials. Sleep. 2015; 38(11):1751-64. DOI:10.5665/sleep.5158. [PubMed]
SHARE THIS ARTICLE
Pain management information, stories and tips accessible anywhere, anytime.
Access clinically supported practical musculoskeletal pain management information to help you understand pain, how you can manage your pain with your management team on the go on any device.